⚠️ How Much Alcohol Is Risky?
About 3–4 drinks per day for men and 2–3 drinks for women over many years increases the risk.
A standard drink equals 12 oz beer, 5 oz wine, or 1.5 oz distilled spirits.
Binge drinking and heavy weekend drinking also contribute.[5]

Symptoms of Alcoholic Hepatitis
Symptoms can vary from mild to severe, often worsening over days to weeks:
- Jaundice (yellowing of skin and eyes due to bilirubin buildup)
- Loss of appetite
- Nausea and vomiting
- Abdominal pain and tenderness in the upper right quadrant
- Fatigue and weakness
- Fever
- Enlarged liver (hepatomegaly)
- Fluid retention in the abdomen (ascites)
- Confusion or altered mental status (hepatic encephalopathy)
- Bleeding from dilated veins (varices) in upper digestive tract in advanced cases
Many patients also suffer from malnutrition and muscle wasting (sarcopenia). Symptoms often appear after heavy drinking or binge episodes but may be subtle early on. Severe cases can rapidly progress to liver failure.[3][4][8][1]
Diagnosis of Alcoholic Hepatitis
Diagnosis relies on:
- Medical history: Long-term heavy alcohol use, recent alcohol intake, symptom onset
- Physical exam: Jaundice, enlarged liver, fluid buildup, signs of chronic liver disease
- Blood tests: Elevated liver enzymes AST and ALT (usually AST/ALT ratio >1.5), raised bilirubin >3 mg/dL, coagulopathy (blood clotting abnormalities), increased white blood cells
- Imaging: Ultrasound or CT to rule out other liver diseases and assess complications
- Liver biopsy: Optional and used if diagnosis is uncertain or to assess severity and guide treatment
Diagnostic criteria also exclude other causes of liver disease such as viral hepatitis or drug-induced injury.
Scores like Maddrey’s Discriminant Function and Model for End-Stage Liver Disease (MELD) help determine severity and prognosis.[4][8][5]

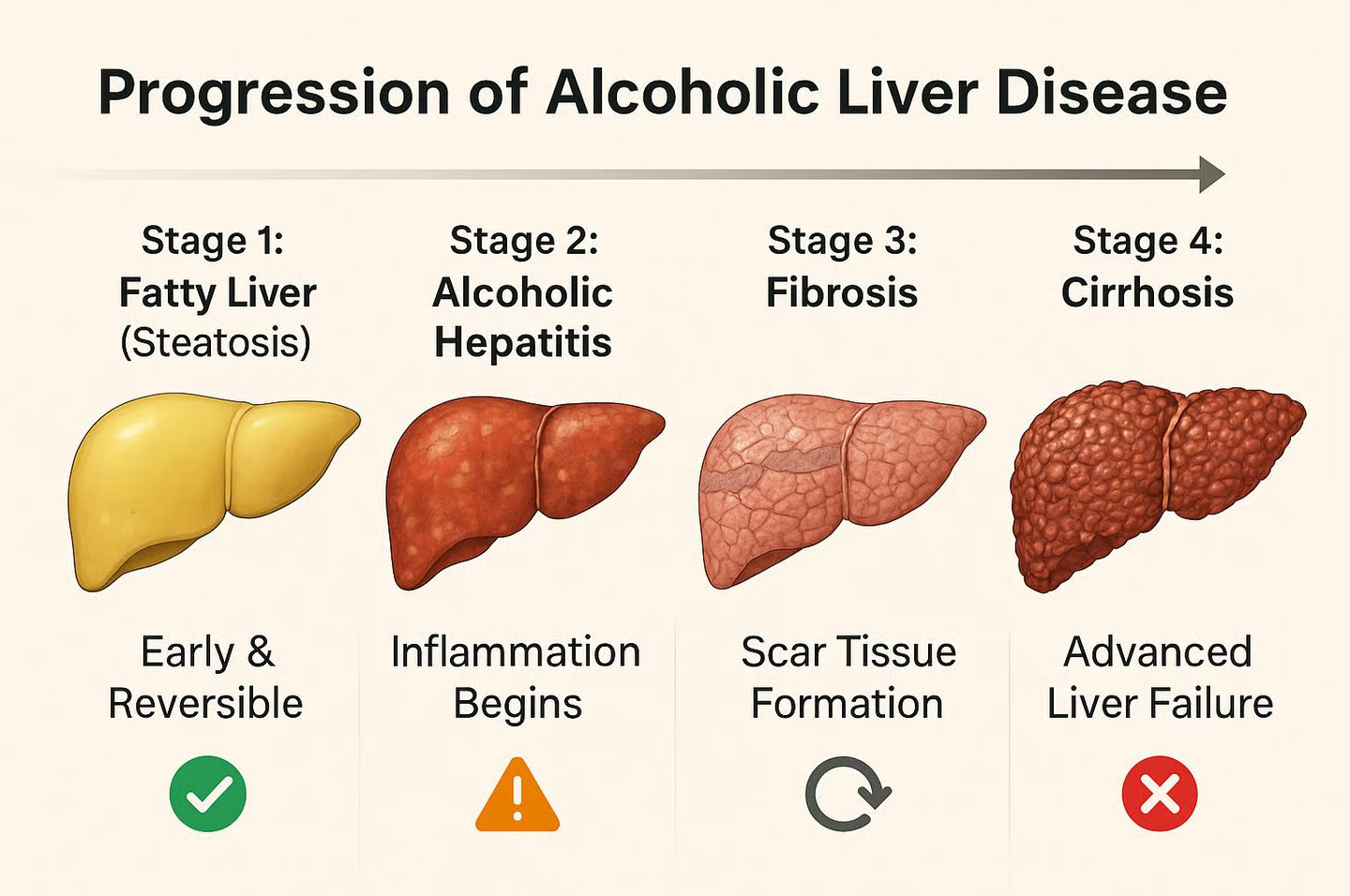
Pathophysiology: How Alcohol Damages the Liver
- Alcohol metabolism primarily occurs via enzymes alcohol dehydrogenase (ADH) and cytochrome P450 2E1 (CYP2E1), producing toxic acetaldehyde.
- Acetaldehyde forms protein and DNA adducts causing direct cell damage.
- Oxidative stress from reactive oxygen species increases inflammation.
- Alcohol disrupts gut lining, allowing bacterial endotoxins into the liver, triggering immune activation.
- Persistent inflammation causes hepatocyte death and liver fibrosis (scarring).
- Fat accumulation (steatosis) also weakens liver cells.
This combination of toxic injury, inflammation, and fibrosis underlies alcoholic hepatitis and can advance to cirrhosis if unchecked.[8][9][3]
Treatment and Management
No specific cure exists; management focuses on:
1. Complete abstinence from alcohol: Essential for recovery and to prevent worsening.
2. Nutritional support: Many patients are malnourished, requiring high-protein diets and vitamin supplementation.
3. Hospitalization in severe cases: For fluid management, treatment of infections, and monitoring.
4. Medications: Corticosteroids like prednisolone may be given in severe alcoholic hepatitis to reduce inflammation but are not universally effective. Pentoxifylline is an alternative if steroids are contraindicated.
5. Symptomatic treatment: Managing complications such as ascites, hepatic encephalopathy, and variceal bleeding.
6. Liver transplant: Reserved for select cases with end-stage liver disease after strict abstinence criteria are met.
Prognosis depends on severity scores and adherence to treatment, with abstinence significantly improving outcomes. Severe alcoholic hepatitis can have high short-term mortality.[2][1][8][5]
Prevention: Reducing the Risk of Alcoholic Hepatitis
- Limit alcohol intake within recommended guidelines.
- Seek help for alcohol dependence early.
- Maintain a balanced diet to reduce malnutrition risk.
- Avoid other liver toxins like certain medications and illicit drugs.
- Regular medical check-ups if heavy drinking is ongoing to monitor liver health.[8]
Frequently Asked Questions (FAQs)
Sources:
[1] Alcoholic Hepatitis https://auctoresonline.org/article/alcoholic-hepatitis
[2] Alcoholic Hepatitis: Diagnosis and Management https://www.binasss.sa.cr/medint/7.pdf
[3] Diagnosis and Treatment of Alcoholic Hepatitis https://pmc.ncbi.nlm.nih.gov/articles/PMC4930399/
[4] ACG Clinical Guideline: Alcoholic Liver Disease – PMC https://pmc.ncbi.nlm.nih.gov/articles/PMC6524956/
[5] Alcoholic Hepatitis: Diagnosis and Management https://www.aafp.org/pubs/afp/issues/2022/0400/p412.html
[6] Alcoholic Hepatitis https://content.ugeskriftet.dk/sites/default/files/scientific_article_files/2018-11/b4755.pdf
[7] Comprehensive Guide to Alcoholic Hepatitis Diagnosis and https://www.coursehero.com/file/245484558/Alcoholic-Hep/
[8] Alcoholic hepatitis (Alcohol-associated hepatitis) https://www.mayoclinic.org/diseases-conditions/alcoholic-hepatitis/symptoms-causes/syc-20351388
[9] Alcoholic hepatitis https://en.wikipedia.org/wiki/Alcoholic_hepatitis
[10] Alcohol-Induced Hepatitis: Symptoms & Treatment https://my.clevelandclinic.org/health/diseases/17853-alcoholic-hepatitis
